BALANCE ASSESSMENT
Balance TrackS (Btracks) is used for balance assessment, fall risk analysis, balance improvement programs, concussion management, Medicare wellness, chiropractic care, physical therapy, vision therapy and balance research
Balance Assessment
BTrackS Assess Balance Software provides protocols for balance assessment and protocols for balance training and rehabilitation. The protocols for assessment include:
• Balance and Fall Risk Assessment – The BTrackS Balance Test (BBT) is a general balance assessment providing detailed postural sway analysis. After each trial, the centimeters of postural sway are calculated and compared to over 20,000 norms to calculate percentile rankings. In addition, a fall risk assessment of Low, Moderate or High is provided with each test result.
• Weight Distribution – Accurately determine weight distribution percentages in the left/right and front/back directions as well as the location of body center of pressure as it relates to global postural alignment.
• CTSIB – The Clinical Test of Sensory Integration and Balance is used to assess how the main three sensory feedback systems for balance (i.e. proprioception, vision, vestibular) function relative to one another. Integrated normative data provides percentile rankings for each of the four trials.
• Limits of Stability – Measure the functional base of support using this biofeedback assessment. Patients stand with feet flat on the plate and lean as far as possible in all directions. The total area, and the area in each quadrant of the plate is calculated in real time.
• Cervical Challenge – Measure postural sway with the patient’s head in 11 different positions. The different positions expose specific vestibular configurations and performance on each trial can be interpreted and utilised by a trained practitioner.
• Single Leg Stance – The Single Leg Stance Test compares the postural sway of an individual when they stand on their left foot versus when they stand on their right foot. When completed, the left-versus-right results are compared and a Symmetry Index is calculated. A person is considered within the Symmetric Range if they show less than 15% difference between right and left.
Why is Balance important?
Balance is an even distribution of weight enabling someone or something to remain upright and steady. A properly functioning balance system allows humans to see clearly while moving, identify orientation with respect to gravity, determine direction and speed of movement, and make automatic postural adjustments to maintain posture and stability in various conditions and activities (1).
Balance is achieved and maintained by a complex set of sensorimotor control systems that include sensory input from vision (sight), proprioception (touch), and the vestibular system (motion, equilibrium, spatial orientation); integration of that sensory input; and motor output to the eye and body muscles (1).
Falls are a major health issue in the community with around 30% of adults over 65 experiencing at least one fall per year. This is set to increase as Australia’s population ages with the proportion of people aged over 65 predicted to increase from 14% (3 million people) in 2010 to 23% (8.1 million people) by 2050. With a stable incidence rate the cost of falls is expected to rise to around $1.4 billion by 2051.
In NSW, the estimated population of people aged 65 and over is expected to rise from 1.27 million people in 2017 to 2.27 million people in 2051, increasing the cost of hip fractures from an estimated $139-209 million in 2017 to $321-482 million by 2051 (2,3,4).
Falls can also result in restriction of activity and fear of falling, reduced quality of life, independence and each fall significantly increases the future risk of not only sprains, strains, and contusions, but also fractures (5). Even falls that do not result in physical injuries can result in the “post-fall syndrome” – a loss of confidence, hesitancy, tentativeness with resultant loss of mobility and independence. It has been found that after falling, 48% of older people report a fear of falling and 25% report curtailing activities. Finally, falls can also lead to disability, decreased mobility which often results in increased dependency on others and hence an increased probability of being admitted to an institution (2).
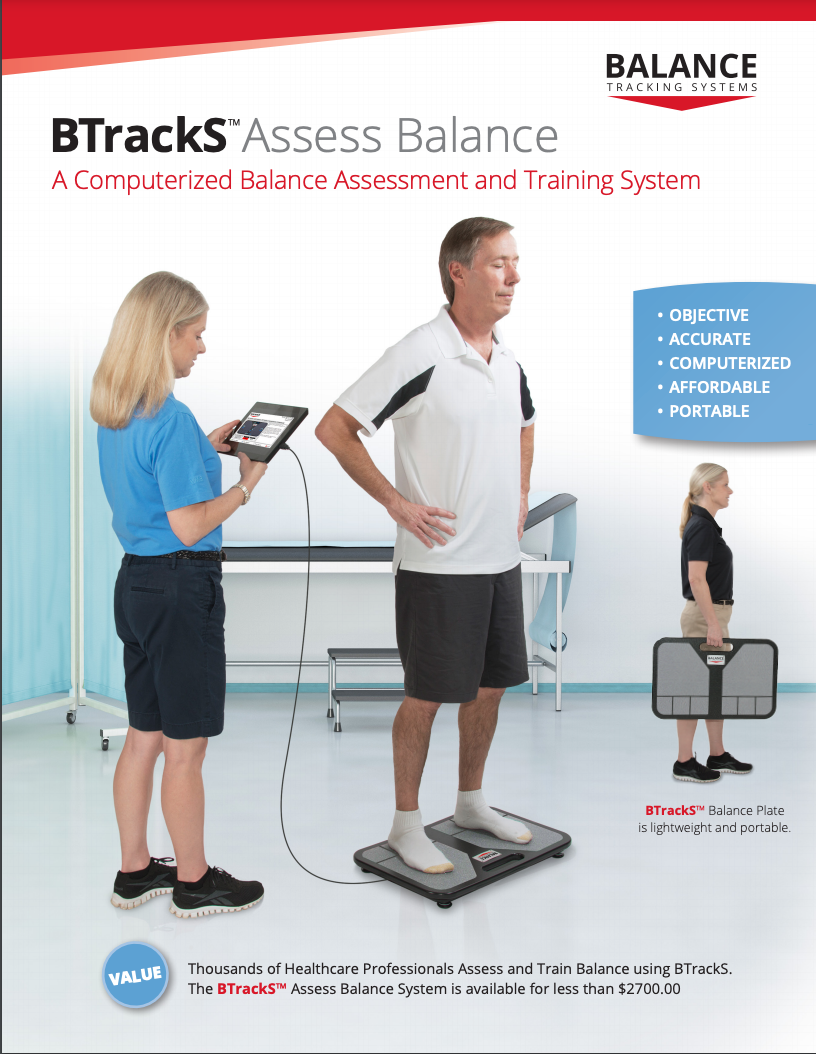
Objectively measuring a person’s ability to maintain their balance using the three different systems (proprioception, visual and vestibular) of balance allows for appropriate interventions and more precise rehabilitation programing. Postural stability can be quantified with measures of vertical and horizontal reaction forces, center-of-pressure (CoP) displacement, or lumbar horizontal displacement. Measures of force and displacement are typically calculated via instruments such as force plates, balance platforms, or accelerometers (8). Here at KC Sports Chiropractic we are currently using the BTrackS (Balance Tracking System) for this very purpose. The BTrackS system allows for analysis of the three balance systems and can be used as a rehabilitation tool as it contains exercises programs to improve certain weaknesses found during the analysis phase.
In conjunction with the BTrackS tool KC also prioritises the use of objective data in other ways to identify and solve issues related to falls and balance. One of the best predictors of a senior citizen falling is toe strength (5). In a prospective study of 300 older adults discovered that non-falling seniors had 20% more toe strength than the seniors who fell (6). Interestingly, there was no difference in quadriceps or ankle strength between the fallers and the non-fallers, confirming that toe weakness, not generalized weakness, is responsible for the falls. Unfortunately, toe weakness is extremely common in senior citizens: compared to their younger peers, older adults have toe strength declines of more than 35%, which greatly increases the risk of falling (7). By improving the strength of the toes many falls and injuries related to falls can be prevented. This approach to preventive rehabilitation care is not limited to the toes. Many strengthening and proprioception training programs have strong evidence to reduce fall injury, minimise fall risk and prevent falls altogether (4).
Sources
VeDA, https://vestibular.org/understanding-vestibular-disorder/human-balance-system
Australian and New Zealand Falls Prevention Society, http://www.anzfallsprevention.org/
Older Australians at a Glance, https://www.aihw.gov.au
Public Health Association of Australia: Policy-at-a-glance – Fall Injury Prevention in Older People Policy.
Thomas C. Michaud, DC, The Importance of Toe Strength in Preventing Falls in the Elderly, https://www.humanlocomotion.org/pages/articles-by-dr-thomas-michaud-1.
Mickle, K, et al., ISB Clinical Biomechanics Award 2009: Toe weakness and deformity increase the risk of falls in older people. Clinical Biomechanics. 2009;24:787-791.
Endo M, Ashton-Miller J, Alexander N. Effects of age and gender on toe flexor muscle strength. Journals of Gerontology. Series A, Biologic Sciences Med Sciences. 2002. 57A(6):M392-397.
Sutton B. Richmond, Kevin D. Dames, Daniel J. Goble, Brett W. Fling, Leveling the playing field: Evaluation of a portable instrument for quantifying balance performance,Journal of Biomechanics 75 (2018) 102–107.